Hyperglycemia Dehydration
Hyperosmolar Hyperglycemic State (HHS): A Dangerous Diabetes Complication
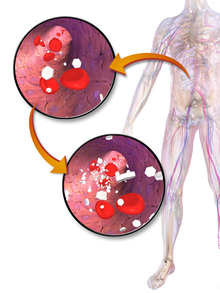
A potentially fatal consequence of diabetes is called hyperosmolar hyperglycemic condition (HHS), formerly known as hyperosmolar hyperglycemic nonketotic coma (HHNC). It develops when blood sugar levels are abnormally high for an extended length of time, which causes severe dehydration and changes in mental state. HHS is less prevalent than diabetic ketoacidosis (DKA), but it has a far greater death rate, thus prompt identification and treatment are essential.
Table of Contents
Recognising the Root Cause: How Does HHS Emerge?
Hyperglycemia Dehydration
HHS mainly affects people with type 2 diabetes, while it sometimes sporadically affects those with type 1 diabetes. The hormone insulin permits cells to take up glucose from the bloodstream and use it as fuel, which controls blood sugar levels in healthy people. Diabetes is characterised by either insufficient insulin production (type 1) or cell resistance to insulin (type 2).
The body tries to excrete extra glucose through urination when blood sugar levels rise as a result of uncontrolled diabetes. This results in frequent urination, which can lead to a substantial loss of fluid. In the event that this fluid loss is not replaced, dehydration occurs.
Hyperglycemia Dehydration
The body in HHS does still manufacture some insulin, albeit not enough to properly control blood sugar, unlike in DKA. The process of breaking down fat for energy, which normally happens in DKA and produces ketones (distinctive byproducts), is prevented by this leftover insulin. Consequently, hyperglycemia (high blood sugar) and hyperosmolarity (abnormally high blood particle concentration) are the hallmarks of haemoglobin HHS, although there is little to no ketosis.
Risk Elements: Who Is Most at Risk for HHS?
Hyperglycemia Dehydration
The following factors raise the chance of developing HHS:
- Diabetes that is poorly managed: People who have uncontrolled type 2 diabetes are most vulnerable.
- Disease or infection: Blood sugar levels can rise and dehydration can be exacerbated by infections, pneumonia, urinary tract infections, and other ailments.
- Medication: Some drugs, such as steroids and diuretics (water pills), can make dehydration and hyperglycemia worse.
- Surgery: The stress of a surgical operation might cause blood sugar levels to rise.
- Dehydration: Situations that restrict the amount of fluid consumed, like extreme heat or vomiting, might make HHS worse.
- Elderly population: People in their latter years may be less likely to recognise dehydration or seek medical assistance right once, especially if they are less mobile or are experiencing cognitive impairment.
- Warning Symbols and Indices: Understanding HHS Understanding HHS takes a few days or weeks to develop. Prompt symptom detection is essential for effective therapy and avoiding consequences.
Observe the following crucial indicators:
Hyperglycemia Dehydration
- Severe thirst and frequent urine: Diabetes is often accompanied by frequent urination, but with HHS: the thirst may be severe and enduring even in the face of frequent urination.
- Severe dehydration: is characterised by dry lips, dry skin, and reduced urine.
- Weakness and weariness: Elevated blood sugar levels can cause weakening and weariness all over.
- Drowsiness and confusion: As dehydration progresses, mental clarity may be compromised, resulting in drowsiness and confusion.
- Seizures or coma: Seizures or coma may result from severe HHS.
Help Seeking: Timely Diagnosis and Intervention Are Critical
Hyperglycemia Dehydration
HHS is a critical health issue. Dial 911 right once if you think someone you know or yourself may have HHS.
Testing for blood osmolality, electrolytes, and sugar levels is part of the diagnosis process for HHS. Typically, treatment entails:
- Intravenous (IV) fluids: In order to treat dehydration and enhance blood flow, prompt rehydration is necessary.
- Insulin therapy: This helps the body utilise glucose again for energy by lowering blood sugar levels.
- Electrolyte replacement: Electrolyte imbalances caused by dehydration must be corrected with intravenous fluids that contain important electrolytes.
- Taking care of fundamental issues: It is imperative to treat any underlying diseases or disorders that may have played a role in HHS.
Stopping HHS: Taking Charge of Your Well-being
Hyperglycemia Dehydration
Although there is no surefire way to totally avoid HHS, there are a number of actions that can greatly lower the risk:
- Effectively control your diabetes: Together with your physician, create a customised diabetes care plan that combines food, exercise, and medication.
- Regularly check your blood sugar levels: Regular blood sugar monitoring enables lifestyle or medication modifications and aids in the early detection of issues.
- Remain hydrated: Even if you don’t feel thirsty, stay hydrated throughout the day by drinking lots of water.
- Acknowledge and treat illness: If you have any infections or diseases that could make your diabetes control worse, get medical help as soon as possible.
- Keep in constant contact with your physician: Make an appointment for routine checkups with your physician to go over diabetes treatment and to determine any possible risks for complications.
Hyperglycemia Dehydration
Diabetes can lead to HHS, a dangerous but avoidable complication. You may greatly lower your risk of developing diabetes by being aware of the symptoms, identifying the risk factors, and using appropriate diabetes management techniques.


