Insulin and Diabetes: Understanding the Key Player in Blood Sugar Control
Share IT

Launch Your Dream Website with Us!
Click Here to Get in touch with Us.
Categories
Role of Insulin in Diabetes
The Secret to Blood Sugar Regulation: Comprehending Insulin’s Function in Diabetes
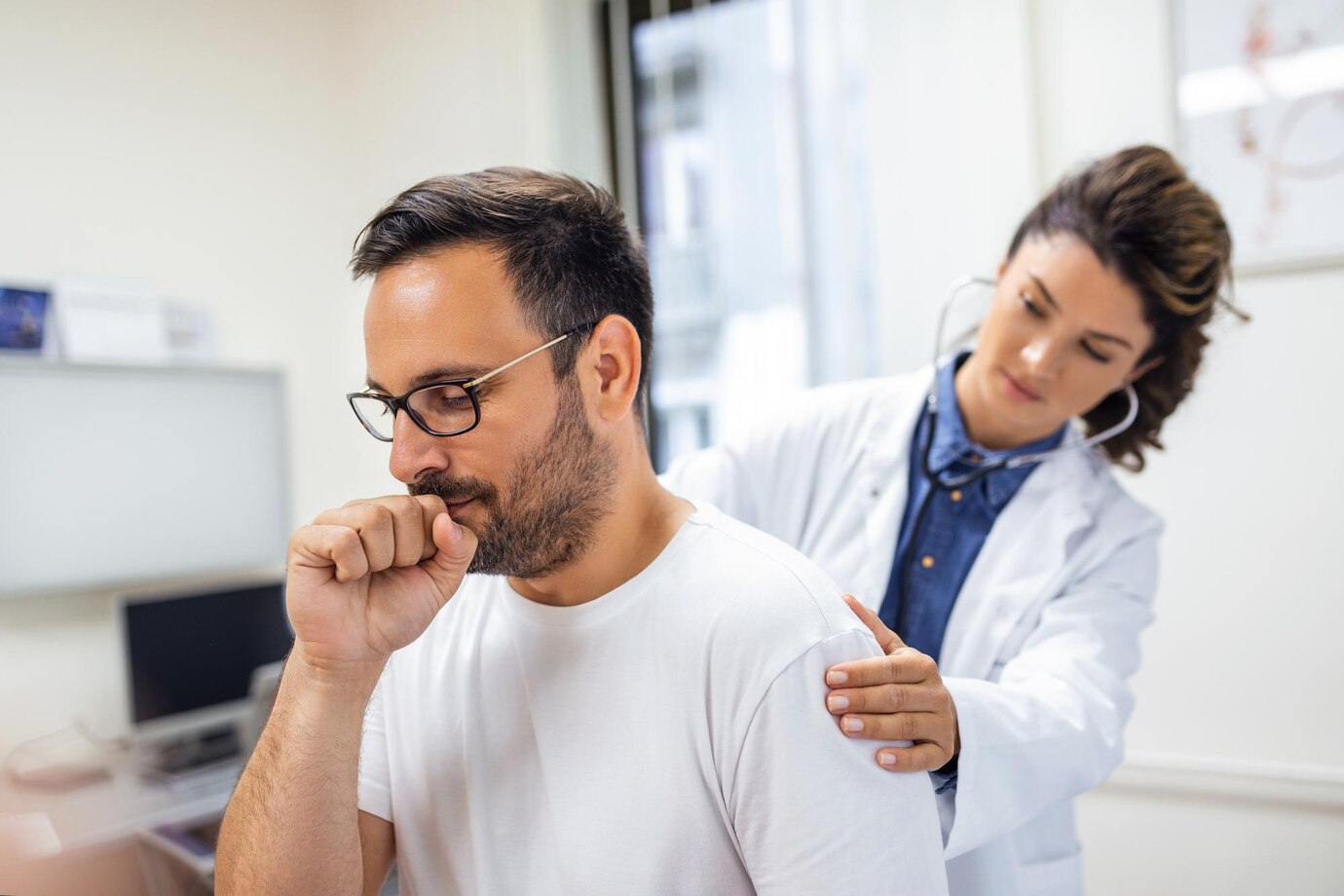
The hormone insulin, which is secreted by the pancreas, is essential for controlling the amount of glucose (blood sugar) in our bodies. But in diabetes mellitus, a chronic illness marked by elevated blood sugar, the insulin system breaks down. This blog post examines the complex interactions between insulin and how various forms of diabetes are caused by disruptions in the hormone.
Thank you for reading this post, don't forget to subscribe!Table of Contents
The Pathway of Insulin Production: From the Pancreas to the Cells
Role of Insulin in Diabetes
Our bodies transform food—particularly carbs—into glucose, which serves as the main energy source for cells. A gland behind the stomach, the pancreas contains unique cell clusters known as islets of Langerhans. Insulin is produced by beta cells located within these islets.
The synthesis and function of insulin happen as follows:
Role of Insulin in Diabetes
- Blood Sugar Rise Following Eating: Our blood sugar levels naturally rise after eating.
- The Insulin-Releasing Pancreas: When blood sugar levels rise, the pancreas detects this change and releases beta cells’ stored insulin.
- The Effect of Insulin on Cells: Insulin functions as a key that opens receptors on body cells all over. As a result, glucose can enter the cells and start producing energy.
- Normal Blood Sugar Levels: Blood glucose levels recover to a healthy range when glucose enters the cells.
The Balancing Act of Insulin: Sustaining Blood Sugar Balance
Role of Insulin in Diabetes
The fundamental job of insulin is to keep blood sugar levels balanced, or homeostasis. It continuously measures and controls blood sugar levels:
- Post-Meal Spike: Insulin facilitates the absorption of glucose into cells and helps control the blood sugar spike that occurs after a meal.
- In-Between Meals: Insulin makes ensuring that cells have a constant supply of glucose to meet their constant energy needs throughout the day.
- Storage for Later Use: Insulin also encourages the liver to transform extra glucose into glycogen, a form of glucose that may be stored, when blood sugar levels are high.
In Case of System Failure: How Diabetes Is Caused by Insulin Dysfunction
Role of Insulin in Diabetes
When this fine balance between the production and action of insulin is upset, diabetes results. There are three primary forms of diabetes, and each is distinguished by unique problems with insulin:
- Type 1 Diabetes: The pancreatic beta cells that produce insulin are accidentally attacked and destroyed by the immune system. Insulin production is thereby completely or almost completely inhibited.
- Type 2 Diabetes: The body either produces insufficient insulin to overcome resistance, or it develops insulin resistance, which causes cells to become less receptive to insulin. At first, the pancreas might try to make up for this by manufacturing more insulin, but eventually, it might not be able to meet the body’s needs.
- Gestational diabetes: Hormonal changes that can impact insulin sensitivity cause this kind of diabetes to develop during pregnancy. It normally goes away after giving delivery, but it raises the chance of Type 2 diabetes in the future.
The Repercussions of Insulin Resistance or Deficiency: High Blood Sugar and Its Consequences
Role of Insulin in Diabetes
Insulin malfunction causes the body to struggle to keep blood sugar levels within normal range in all forms of diabetes. If untreated, this persistent hyperglycemia (high blood sugar) can result in a number of problems, such as:
- High blood sugar: damages blood arteries and raises the risk of heart disease and stroke, two cardiovascular problems.
- Damage to the nerves: also known as neuropathy, can result in pain, weakness, tingling, and numbness, especially in the legs and feet.
- Nephropathy, or kidney disease: Excessive blood sugar can harm the kidneys and cause renal failure.
- Diabetes: can harm the blood vessels in the retina, which may result in visual impairments (retinopathy).
- Foot issues: Infections and foot ulcers can be exacerbated by poor circulation and nerve loss, and in extreme situations, amputation may be necessary.
Taking Care of Diabetes with Insulin and Lifestyle Changes
Role of Insulin in Diabetes
Insulin injections are an essential part of blood sugar management, even though there is no known cure for Type 1 diabetes. Treatment for Type 2 diabetes often consists of a combination of dietary changes, physical activity, and weight control. Medication, such as insulin injections, may also be required in some circumstances.
Role of Insulin in Diabetes
Knowing how insulin functions and how diabetes results from it gives people the power to take charge of their health. Effective diabetes treatment and lowering the risk of complications require collaborating with healthcare providers and implementing healthy lifestyle choices.

Launch Your Dream Website with Us!
Click Here to Get in touch with Us.




















































Recent Comments